Many environmental factors have been associated with the development of autoimmunity.1 Infections, for example, can cause reactive arthritis by triggering a (genetically) predisposed immune system.2 Smoking, in a similar, but arguably different, way, can trigger the production of autoantibodies by inducing citrullination of proteins.3,4 Exposure to silica dust, which is a crystalline derivate of quartz commonly found in construction materials and mining activities, has been shown to cause a very peculiar pulmonary inflammation in patients with rheumatoid arthritis (RA).5 Furthermore, physical distress or infections can reactivate a quiescent rheumatic disease.6 Similarly, environmental air pollution has been associated with the development of autoimmune diseases and, more recently, with higher risk of disease flare.7–12
Air pollution is a major cause of death worldwide and increasing evidence show that air pollution can increase the incidence of rheumatic musculoskeletal diseases (RMDs). The present review discusses the effect of airborne environmental pollution on several rheumatic diseases. Moreover, it focuses on the most widely used approaches for the assessment of air pollution and the effects of chronic and acute exposure on the risk of developing a rheumatic disease.
Investigating the exposure to air pollution
Investigating the association between exposure to air pollution and health outcomes might be challenging. Biases relating to exposure assessment and population selection can affect the research.13 The measurement of air pollutants is often complicated, and linking the exposure to individuals is not straightforward. The most common methods and their limits are listed in Table 1.
Table 1: Approaches for measuring exposure to air pollution
|
Methods |
Advantages |
Limitations |
Examples of pollutants measured |
|
Air quality monitors |
Vast area of analysis, detailed daily exposure data, sampling of various pollutants (gaseous and particulate) |
Misclassification bias, influenced by weather conditions |
PM (e.g. PM2.5 or PM10), carbon monoxide (CO), nitric oxide (NO), nitric dioxide (NO2), oxides of nitrogen (NOx), ozone (O3) |
|
Exposure modelling |
Vast area of analysis, detailed daily exposure data |
Misclassification bias |
Most models explore PM |
|
Geostationary satellites |
Vast area of analysis, controls for weather conditions |
Misclassification bias, not easily accessible, usually limited to PM |
Most models explore PM |
|
Personal devices |
Precise assessment of personal exposure |
Costs, usually limited to PM, Hawthorne effect |
Most devices explore PM |
|
Indoor/outdoor sampling |
Precision and various pollutants analyzed |
Costs, Hawthorne effect |
PM (e.g. PM2.5 or PM10), carbon monoxide (CO), nitric oxide (NO), nitric dioxide (NO2), oxides of nitrogen (NOx), ozone (O3) |
|
Biological markers |
Precise assessment of personal exposure, reflect biological effects on health |
Costs, usually measure cumulative exposure |
Heavy metals (such as cadmium, mercury, lead etc.), perfluorohexane sulfonate (PFHxS), perfluorooctane sulfonate (PFOS), perfluorononane sulfonate (PFNS), perfluorooctanoate (PFOA), perfluorononanoate (PFNA), perfluorodecanoate (PFDA), benzopyrene, etc. |
PM = particulate matter.
One method for assessing exposure to air pollution is via air quality monitors.13 Air quality can be monitored by establishing stations over a certain territory. Thousands of such air quality stations are spread across Europe and the United States. This method represents, by far, the most common approach for assessing chronic and acute exposure to air pollution. Patients’ data are linked to air quality data through zip code centroids, which can be smaller or larger depending on the precision required. However, such an approach might lead to misclassification (i.e. incorrect linking between patients and exposure to air pollutants) and be inaccurate in measuring personal exposure.13 For example, patients can relocate and commute to work. Moreover, the data may be influenced by wet deposition, a phenomenon caused by precipitation to the ground of coarse particulate matter (PM) by the rain.14 Similarly, geospatial models, which use data from geostationary satellites measuring dispersed PM on the surface of the Earth, may also be imprecise.15 Nonetheless, there are various countermeasures that can be applied to reduce these biases. For example, questionnaires on personal exposure to air pollution and on life and commute habits could help to refine the exposure data. Moreover, many statistical models can now control for weather conditions (e.g. rain or wind).16
Personal devices represent another approach to exposure assessment.17 A variety of monitors are available, from research grade to cheaper commercial instruments.18 Most of these devices can only measure PM, and their precision and accuracy might not be satisfactory. Nevertheless, this approach gives the best estimate of personal exposure and quantifies both household and outdoor exposure to air pollution. However, compliance might be scarce, and studies might be limited by a small number of subjects. Moreover, these studies might be affected by the Hawthorne effect.19 Indeed, subjects that wear personal devices may tend to modify their behaviour toward a ‘greener‘ attitude by avoiding exposure to sources of pollutants.
A more cumbersome method for determining exposure to air pollution is through the direct measurement of certain biological markers in human samples (e.g. blood or urine).20 For example, benzene or benzo-pyrene can be easily measured in frozen urine.20 Although this approach is possibly the most precise in terms of personal exposure estimation, it is limited by several factors. First, it can only provide a measurement of cumulative exposure, whose length is related to the half-life of the end-product tested. Second, it has intrinsic costs, and research–grade facilities and laboratories are needed to perform the analyses.
On the other hand, assessing the effects of either chronic or acute exposure to air pollution on health outcomes is more complicated. To study the long-term effects of air pollution on health outcomes, we need a methodology that can measure the quality of the air over a long time. Currently, air sampling (i.e. through air quality station monitoring) is the only methodology that can estimate long-term exposure. However, systematic measurements of airborne pollutants were first started in the 1980s and 1990s; therefore, we can only roughly estimate the lifelong exposure to certain pollutants. Indeed, in most studies, long-term exposure is extrapolated from a certain time window, which serves as a proxy for long-term exposure.13,15,16 However, such approximation might result in misclassification due to, for example, the relocation of patients. We can also explore the effects of acute exposure to high levels of air pollution on health-related events. A case-crossover design can be applied to explore how transient exposure affects the risk factors of an acute-onset disease.21 Indeed, brief exposures might cause a transient change in the risk of disease reactivation (i.e. flares). In case-crossover studies, instead of obtaining information from two groups (i.e. cases and controls), the exposure information is obtained by comparing two different periods of time in the same group of patients followed longitudinally. This approach enables control of between-patient confounders and within-patient time-invariant confounders. Typically, conditional logistic regression is applied to case-crossover studies to control for time-varying confounders (e.g. variations in medication, infections).22
In the following paragraphs, the effects of both types of exposures, chronic and acute, on RMDs are reviewed.
Chronic exposure and risk of rheumatic musculoskeletal diseases
According to a recent report by the World Health Organization, air pollution exposure is a major determinant of mortality and morbidity worldwide.23 Exposure to air pollution has been linked to a higher risk of major cardiovascular events, pulmonary diseases and cancer.24–28 In addition, growing evidence supports the role played by chronic exposure to airborne toxins derived from fossil combustion in causing various immune-mediated conditions.7–12 It was shown that the immune system can be triggered by exposure to environmental stimuli, including airborne pollutants.3 Numerous preclinical studies have found that exposure to heavy metals, fine PM and gaseous pollutants can harm lymphocytes.29–32 Inhalation of pollutants stimulates the the bronchus-associated lymphoid tissue to produce pro-inflammatory cytokines and, more importantly, autoantibodies.33
The first and probably most notable example of such association comes from the observed relationship between silica dust exposure and RA.5 In the 1950s, it became clearer that patients with RA were more susceptible to exposure to silica dust. Indeed, patients with RA tend to develop pulmonary inflammatory nodules, whose inflammation is histologically similar to synovitis.34 More recently, further support has been gathered on the key role played by the environment in the development of RA. Data from the Swedish population-based case–control study showed that occupational exposure, smoking and genetics work together to increase the risk of developing anticitrullinated protein antibodies (ACPA)–positive RA.35 Smokers with a certain genetic background exposed to gasoline engine exhaust had an 18-fold higher risk of developing RA. Interestingly, the origin and nature of the pollutant seem to be only partially related to the higher risk. Indeed, even exposure to hard rock (e.g. uranium, zircon, gold) has been associated with a higher risk of developing RA. Blanc et al. showed that miners and individuals exposed to hard rock mining activities had nearly four times the risk of RA.36 Interestingly, miners were also at risk of other non-RA arthritides, underlining that dust exposure has a holistic effect on the immune system. Similarly, soldiers exposed to burn pits had a greater risk of presenting ACPA–positive RA.37 Finally, chronic exposure to fine PM has been linked to a higher risk of RA and other RMDs and immune-mediated diseases (IMIDs).7
The magnitude of the effect of air pollution exposure should not be underestimated. Chronic exposure to concentrations of PM2.5 (i.e. of less than 2.5 μm) above 20.0 μg/m3 has been associated with a 13.0% higher risk of developing an autoimmune disease (adjusted odds ratio 1.128, 95.0% confidence interval [CI] 1.056–1.205); this risk was even higher for RA (adjusted odds ratio 1.559, 95.0% CI 1.401–1.734).7 Notably, the annual average PM2.5 concentration limit of 20.0 μg/m3 is exceeded in many industrialized regions across Europe and the World.23 A remarkable example of this is the Po Valley, in Northern Italy, where the average concentration of PM2.5 was as high as 25.0–30.0 μg/m3 in 2021.28
In summary, chronic exposure to a variety of pollutants has been associated with a higher risk of IMIDs. Vitamin D may explain this empirically proven association. Indeed, UVB with a wavelength of between 290.0 and 315.0 nm convert cholesterol in the skin into vitamin D,37,38 whose administration, as further demonstrated by a recently published large randomized controlled trial,39 has been associated with a lower probability of developing autoimmune diseases.40 However, aero-dispersed PM can block UVB radiation intensity on the ground. Interestingly, UVB with a wavelength above 150.0–200.0 nm cannot even reach the ground when the concentrations of PM10 (i.e. of 10.0 μm or less) are above the World Health Organization threshold for human health protection, largely impairing the skin‘s vitamin D production.41,42 In addition, there is evidence suggesting that exposure to UVB light is linked to a lower risk of RA.43 The reasons behind this connection are not yet clear, but it could be due to its role in producing vitamin D. However, whilst some studies have shown a connection between sunlight exposure and reduced risk of RA,43,44 Zhao et al. did not demonstrate a clear correlation between sun exposure or sun–block use and ACPAs.45 However, the same authors found a significant relationship between industrial PM2.5 emissions and ACPAs.45,46 Further studies are needed to determine the exact role of UVB exposure and/or vitamin D on RA and inflammatory RMD risk.
RA is paradigmatic of how air pollution can affect the immune system. However, air pollution has been shown to affect a variety of other IMID–related diseases, such as systemic lupus erythematosus (SLE) and systemic sclerosis. For example, silica dust exposure has been associated with both systemic sclerosis and SLE.47 Silica dust is a well-established adjuvant that can promote the expression of pro-inflammatory cytokines, enhance T cell responses, reduce the number of regulatory T cells, increase oxidative stress and cause apoptosis.48,49 The association between SLE and silica dust exposure has been studied extensively,50–55 indicating that exposure to crystalline silica may increase the likelihood of SLE in some individuals. Again, silica dust has been associated with poor prognosis of systemic sclerosis and with younger age at diagnosis.47 Air pollution exposure is also the cause of relevant comorbidities that affects patients with inflammatory RMDs. Interstitial lung disease (ILD) is almost certainly the most relevant among these conditions. In a paper published in 2022, Zhao et al. monitored 280,516 patients who developed RA for the first time and identified 2,194 cases of RA-ILD across 1,394,385 persons per years.56 Their analysis showed that the risk of RA-ILD onset increased by 1.54 times (95.0% CI 1.47–1.63) for every 10.0% increase in exposure to the seven pollutants studied. Of the PM2.5 components, ammonium, mineral dust and black carbon were found to have a greater impact on ILD risk compared with the other components.
Acute exposure to air pollution and risk of flares
Acute exposure to high levels of pollutants has been shown to increase the risk of myocardial infarction, stroke, asthma and chronic obstructive pulmonary disease exacerbations and numerous other acute-onset conditions.57–59 Indeed, exposure to high levels of toxic components of air pollution has been shown to acutely stimulate the immune system toward a pro-inflammatory status.60 During highly polluted days, an increase in serum concentrations of C-reactive protein was demonstrated.61
In recent years, there has also been growing evidence of the acute effect of air pollution on the risk of reactivation of several RMDs. For example, a study on 888 patients with RA followed for more than 5 years showed an exposure-response relationship between the concentration of air pollutants and the risk of having abnormal C-reactive protein levels.8 In addition, patients exposed to greater concentrations of air pollutants were at higher risk of having arthritis flares. The same result was replicated in another cohort of patients with RA exposed to high levels of pollutants.62 Similarly, a third study showed that acute exposure to air pollution was associated with biological disease–modifying anti-rheumatic drug switches in patients with inflammatory arthritides.9 Furthermore, exposure to acute levels of pollutants was associated with psoriasis and lupus reactivations.10,63 More recently, a study showed that exposure to gaseous pollutants and particulate matter may trigger SLE nephritis.64
Interestingly, a detrimental, acute effect of exposure to air pollution was also noted in non-inflammatory (at least prevalently non-inflammatory) conditions such as osteoporotic fractures.65,66 Whilst a negative effect on the bone from chronic exposure to air pollution is reasonable and largely supported by preclinical and empirical studies,65,66 an acute effect on fracture risk is somehow tougher to explain. Indeed, bone fragility is generally considered a chronic disease that develops over a long period whose culprit, the fracture, tends to happen after a fall. Therefore, it is tougher to explain an acute role of air pollution on bone, which is a relatively stable tissue. Nonetheless, a 2018 study showed a short-term temporal relationship between air pollution exposure and hip fragility fractures.67 More recently, a very similar finding was demonstrated in more than 1,000 hip fragility fractures.68 In both studies, the authors hypothesize that the association between air pollution exposure and fracture risk may mostly be explained by a higher fall risk, which might be caused by acute exposure to air pollution. Interestingly, when the results were stratified by age, this relationship remained true only in older patients. Indeed, acute exposure might be one of the culprits of chronic damage that persisted over the years. The latter speculation might also apply to RMDs and the risk of flares.
Conclusions
Environmental air pollution and climate change represent major health and societal challenges. More than 7 million people die every year due to air pollution, and most of these deaths would be preventable with a slight reduction of fossil combustion emissions.23,27,28 The environment plays a crucial role in the pathogenesis of RMDs; most of the evidence produced has concerned RA, but emerging studies have found a similar relationship in other autoimmune diseases. In addition, acute exposure to high levels of airborne pollutants poses a risk of flaring of RMDs. Again, this association was first demonstrated in patients with RA but is now clearer in other conditions, such as psoriasis or SLE.
Research on the relationship between air pollution exposure and autoimmune diseases is an active area of investigation. In recent years, several studies have explored the connection between air pollution and autoimmune diseases. These studies have shown that exposure to air pollutants, such as PM, nitrogen dioxide (NO2) and ozone (O3), can have an impact on the immune system and increase the risk of autoimmune diseases. The exact mechanisms by which air pollution contributes to the development of autoimmune diseases are not fully understood; however, they likely involve the activation of pro-inflammatory cytokines, oxidative stress and changes in the number and function of immune cells (Figure 1). Despite the advances in our understanding of the relationship between air pollution exposure and autoimmune diseases, much work remains to be done. Future research in this area should focus on characterizing the effects of specific air pollutants and their mixtures on the immune system, understanding the individual and environmental factors that influence susceptibility to air pollution-induced autoimmune diseases, and exploring the underlying biological mechanisms linking air pollution and RMDs. Additionally, research should also examine the effectiveness of interventions, such as air pollution control measures and lifestyle changes, in reducing the risk of autoimmune diseases in individuals exposed to air pollution.
Figure 1: Effects of air pollution exposure on inflammatory rheumatic musculoskeletal diseases
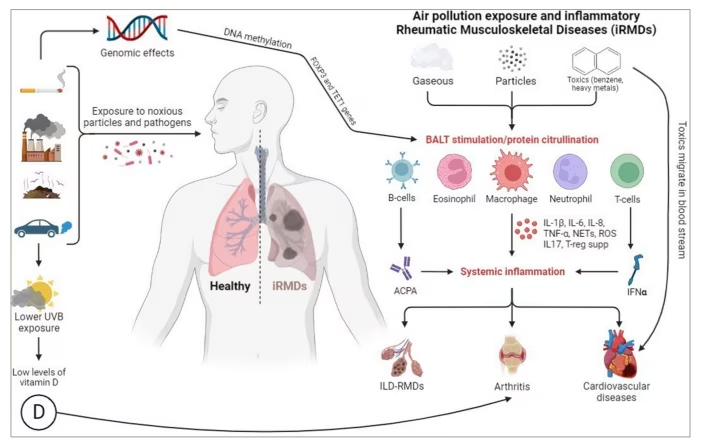
ACPA = anticitrullinated protein antibodies; FOXP3 = forkhead box P3; IL = interleukin; ILD = interstitial lung disease; IFNα = Interferon alfa; iRMDs = inflammatory rheumatic musculoskeletal diseases; NETs = neutrophil extracellular traps; RMDs = rheumatic musculoskeletal disease; ROS = reactive oxygen species; supp = suppression; TET1 = translocation methylcytosine dioxygenase 1; TNF-α = tumour necrosis factor alpha.