The global burden of disease is heavily impacted by the increased prevalence of chronic inflammatory rheumatic diseases (CIRDs [rheumatoid arthritis (RA), spondyloarthritis (SpA), connective tissue diseases (CTDs) crystal arthropathies and polyarticular osteoarthritis (OA)]), which are prevalent chronic non-communicable diseases associated with pain, functional impairment, and years lived with disability (YLDs).1–4
Comorbidities associated with CIRDs contribute significantly to the disease’s impact on patients’ lives, including long-term impairment, frequent use of healthcare, worse functional status, lower quality of life, and higher mortality.2,4 Comorbidities such as cardiovascular disease have an increased incidence in patients with CIRDs, which is often explained by the disease’s activity, its treatment, or by increased susceptibility to risk factors such as smoking, high blood pressure and hyperlipidaemia.2,5,6 Some comorbidities may also restrict therapeutic alternatives, affecting treatment plans and jeopardising optimal treatment outcomes.5–7
Additionally, screening for comorbidities in patients with CIRDs tends to be less systematic than in the general population, primarily because the emphasis is placed on managing their rheumatic disease.7 The most frequent comorbidities in general and in CIRD populations are cardiovascular diseases and cardiovascular risk factors, malignancies and depression, where screening recommendations are currently published.8–15 In addition, the European Alliance of Associations for Rheumatology (EULAR) recommends screening for osteoporosis, infections and gastrointestinal diseases in patients with CIRDs.7
In this narrative review, we summarize the current recommendations for screening and managing comorbidities in patients with CIRDs. We also highlight the impact of comorbidities on the selection of disease-modifying anti-rheumatic drugs (DMARDs).
Methods
Narrative literature review
To gather published recommendations on reporting, screening for, or prevention for each of the chosen comorbidities (cardiovascular diseases, malignancies, infectious comorbidities, gastrointestinal diseases, osteoporosis and depression), a literature review was carried out in July 2023. All information was extracted from PubMed using a research equation based on the Patient, Intervention, Comparison, Outcome (PICO) model (Supplementary Table 1).16 The literature search identified 325 articles (Supplementary Figure 1). Based on the title and the abstract, we assessed 123 full-text articles for eligibility. Moreover, we excluded 50 articles since they were written in a language other than English, had out-of-date recommendations, or did not fit the inclusion requirements for the study. Consequently, 73 articles were included in this narrative review, and 27 articles related to pulmonary comorbidities and obtained by cross-referencing were subsequently added.
Target population
The target population for this study is all patients with CIRDs comprising of RA, SpA, CTDs and crystal arthropathies, as well as patients with other musculoskeletal diseases including OA.
Choice of selected comorbidities
The choice of comorbidities for this review was based on the Comorbidity Collecting Form from the 2016 EULAR initiative.7 The criteria for these comorbidities were as follows: cardiovascular diseases (CVD) including myocardial infarction, angina, stroke, transient ischaemic attack, heart failure and lower limb peripheral arterial disease; malignancies including lymphoma, skin, lung, colon, breast, and cervical cancers; infections including serious infections, chronic viral infections, tuberculosis (TB) and non-TB opportunistic infections; gastrointestinal (GI) diseases including gastroduodenal ulcers, osteoporosis and depression.2,3,5–7 In addition, articles related to important comorbidities not included in the EULAR initiative, such as interstitial lung diseases and pulmonary arterial hypertension, were subsequently incorporated.
For each selected comorbidity, the major epidemiologic features and the current screening and management guidelines in patients with CIRDs were presented. In addition, the impact of comorbidities on the selection of DMARDs was discussed.
Results
The following data was retrieved from each selected article published between 2016 and 2022: definition of the comorbidity, how to document its presence, suggested screening method, and screening interval. For recommendations on reporting of, screening for, or prevention of each of the selected comorbidities in the general population, we referred to USPSTF’s and CDC’s databases.
Cardiovascular risk factors and diseases
Patients with CIRDs frequently underestimate the cardiovascular component of their illness, which can make managing their CVD comorbidity challenging.17 Nonetheless, due to both established and emerging risk factors including systemic inflammation and autoimmune dysregulation, patients with CIRDs have an elevated risk of CVD.18,19 Any component of the cardiovascular system can be impacted.20 CVD is the leading cause of mortality among patients with CIRDs, which can go up to 50% higher in patients with RA compared with the general population.21 Additionally, patients with RA are more likely to have silent ischaemic disease, which can result in unexpected deaths, further complicating the screening process within this population.22
Recommendations from the World Health Organization (WHO) and EULAR 2016 task force on CVD risk management in patients with CIRDs agree that rheumatologists should screen for risk factors and implement management plans with their patients.19,23 An example of this would be encouraging lifestyle changes, including adopting a healthy diet by reducing consumption of high-calorie foods and increasing fruit and vegetable intake, engaging in regular moderate-intensity exercise for at least 150 min per week with particular emphasis in patients with OA and axial spondyloarthritis (axSpA), as well as smoking cessation, as tobacco has detrimental effects on symptoms, disease activity, progression, comorbidities and response to DMARDs.19,23–26
As for screening, in addition to screening those with traditional risk factors (Table 1), patients diagnosed with CIRDs, especially RA, axSpA or psoriatic arthritis (PsA), should undergo CVD risk assessment at least once every 5 years.9,10,12–14,17,19,21,27–42 If the initial assessment indicates a low risk, routine screening after 5 years is recommended. However, rescreening may be done sooner if the risk is intermediate or disease progression is rapid. Patients with a high risk or established CVD should be treated for existing risk factors according to existing guidelines. Furthermore, it is essential to reassess CVD risk after significant changes in anti-rheumatic therapy, particularly when initiating biological DMARDs or other medications that may significantly affect lipid levels or other CVD risk factors.19
Table 1: Optimal screening and management of comorbidities and risk factors in patients with chronic inflammatory rheumatic diseases9,10,12–14,17,19,21,27–43
|
Comorbidity/risk factor |
Eligible patients |
Optimal screening |
Optimal management |
References |
|
Hypertension |
Patients with RMD older than 18 years |
Blood pressure yearly |
Refer for treatment if >140/90 mmHg |
USPSTF10/EULAR19 |
|
Diabetes |
Patients with RMD older than 40 years |
Free blood sugar or HbA1c or oral glucose tolerance test every 3 years |
Refer for treatment if HbA1c 6.5% or higher |
USPSTF27/EULAR19 |
|
Hyperlipidaemia |
Patients with RMD: men older than 35 years; women older than 45 years |
Lipid profile every 5 years |
Start statin if LDL >or = to 0.7 g/L |
USPSTF28/EULAR19 |
|
Atherosclerosis |
Patients with RMD |
Carotid ultrasound |
Start statin if presence of carotid plaque |
EULAR19 |
|
CVD risk factors (all of the above + smoking) |
Patients with RA, axSpA and PsA |
mSCORE every 5 years |
Low risk: repeat in 5 years Intermediate risk: repeat in less than 5 years High risk: treat |
17,21,29 |
|
Breast cancer |
Women between 50–74 years |
Biennial mammogram |
Refer to specialist |
USPSTF13 |
|
Cervical cancer |
All women |
Cervical smear test every 3 years |
Refer to specialist |
USPSTF30 |
|
Lymphoma |
Patients with SjS and RA |
No clear recommendations, regular follow-ups with primary physician |
Refer to specialist |
|
|
Lung cancer |
Smokers or past smokers aged 50–80 |
Low-dose thoracic CT scan yearly |
Refer to specialist |
USPSTF9,31 |
|
Colorectal cancer |
All adults between 50–75 years |
Colonoscopy every 5–10 years or gaiac-based faecal occult blood test every 2 years |
Refer to specialist |
USPSTF12 |
|
Influenza |
Patients with RMD |
N/A |
Yearly vaccination |
CDC32/EULAR33,34 |
|
Pneumococcus |
Non-vaccinated pediatric patients with RMD; patients with RMD older than 65 years; patients who are prescribed biologics and/or high doses of GCs |
N/A |
Vaccination every 5 years |
CDC35/EULAR36,37 |
|
HPV |
Women between 18–26 years |
Cervical smear test, every 3 years |
Refer to specialist |
CDC35/EULAR37 |
|
VZV |
Patients starting csDMARDs, bDMARDs, tsDMARDs, immunosuppressants, and/or high dose GCs non-immune to VZV |
N/A |
Post-exposure prophylaxis following contact with VZV |
EULAR38 |
|
HBV |
Patients with RMD prior to bDMARDs, tsDMARDs, immunosuppressants, and high dose GCs |
HbSAg |
Refer to specialist |
USPSTF39/EULAR38 |
|
HCV |
Patients with elevated alanine aminotransferase levels or known risk factors, before initiating these medications |
Anti-HCV antibody testing and PCR |
Refer to specialist |
USPSTF40/EULAR38 |
|
HIV |
All patients between 15–65 years |
Antigen/antibody immunoassay |
Refer to specialist |
CDC35/EULAR41 |
|
Tuberculosis |
Adults 18 years and older at high risk |
Interferon-gamma release assay preferably, or tuberculin skin test and chest X-ray |
Refer to specialist |
USPSTF42/EULAR41 |
|
SARS-CoV-2 |
Patients with RMD |
PCR |
Vaccination: 1–3 doses separated by at least 3–4 weeks. Vaccine booster based on physician’s judgment |
CDC32 |
|
Osteoporosis |
All adults 65 years and older; all patients with RMD; or presence of fragility fracture |
DXA at least once |
No primary prevention except in long term GCs |
USPSTF31 |
|
Depression |
All adults (evidence currently insufficient for adolescents aged 12-18 years)43 |
Clinically and based on scores |
Refer to specialist |
USPSTF14 |
axSpA = axial spondyloarthritis; bDMARDs = biologic disease-modifying anti-rheumatic drugs; CDC = Centers for Disease Control and Prevention; csDMARDs = conventional synthetic disease-modifying anti-rheumatic drugs; CT = computed tomography scan; CVD = cardiovascular disease; DXA = dual-energy X-ray absorptiometry; EULAR = European Alliance of Associations for Rheumatology; GCs = glucocorticoids;HbA1c = glycated haemoglobin; HbSAg = hepatitis B surface antigen; HBV = hepatitis B virus; HCV = hepatitis C virus; HIV = human immunodeficiency virus; HPV = human papillomavirus; LDL = low-density lipoprotein; mSCORE = Modified Score for Cardiovascular Risk; N/A = not applicable; PCR = polymerase chain reaction; PsA = psoriatic arthritis; RA = rheumatoid arthritis; RMD = rheumatic and musculoskeletal diseases; SjS = Sjögren’s syndrome; tsDMARDs = targeted synthetic disease-modifying anti-rheumatic drugs; US = ultrasound; USPSTF = United States Preventive Services Task Force; VZV = varicella-zoster virus.
CVD risk assessment in patients with CIRDs is done by using the Systematic Coronary Risk Evaluation index (SCORE) coupled with the modified SCORE (mSCORE), as recommended by EULAR.19,21 Indeed, these risk indexes specifically tailored for patients with RA are more specific than scores used in the general population, such as the Framingham score or SCORE alone, which tend to underestimate CVD risk in patients with RA, especially older individuals, those who are rheumatoid factor (RF) positive, and those with high levels of inflammation.17,29
Screening methods used to assess cardiovascular involvement in patients with CIRDs are often the same as those used in the general population, such as echocardiography, chest X-rays, and electrocardiograms.44 Additional techniques may be utilised for further assessment – for instance, carotid ultrasound can be employed to screen asymptomatic atherosclerotic plaques in individuals with RA.45,46 Carotid magnetic resonance imaging, cardiac magnetic resonance, and serum calprotectin have also been suggested as potential screening tools for CVD risk factors, myocardial inflammation, ischaemia and fibrosis, to respectively complement carotid ultrasound, assess cardiac involvement in systemic lupus erythematosus (SLE) and RA, and serve as a biomarker for subclinical atherosclerosis in Sjögren’s syndrome.20,46,47
As for the management of CVD risk in patients with CIRDs, it closely resembles that of the general population.48 The Early Rheumatoid Arthritis COR Intervention (ERACORI) protocol proposes a unified management plan based on Danish national guidelines for CVD management, recommending prescription of angiotensin-II receptor antagonist as the preferred antihypertensive drug at the maximal dose, as well as statins, starting with an initial treatment of 40 mg simvastatin, which can be adjusted to 80 mg atorvastatin or supplemented with ezetimibe 10 mg if necessary, aiming to achieve an LDL cholesterol level below 2.5 mmol/L.49
There has been a positive correlation between the use of anti-inflammatory medications like nonsteroidal anti-inflammatory drugs (NSAIDs) and glucocorticoids (GCs) in patients with RA and the increase in CVD risk (Figure 1).24 Indeed, GCs were associated with CVD risk factors and mortality, but they may also have a beneficial effect in reducing CVD risk through inflammation control.18,24 As for NSAIDs, they were shown to increase CVD risk in RA, even though the PRECISION (Prospective randomized evaluation of celecoxib integrated safety vs ibuprofen or naproxen; ClinicalTrials.gov identifier) trial found an acceptable CVD safety profile for some NSAIDs such as celecoxib, ibuprofen and naproxen.50 Other anti-rheumatic therapies like methotrexate (MTX) and tumour necrosis factor inhibitors (TNFi) were associated with a reduced CVD risk as they can slow down the progression of arterial thickness.18,24,51 However, concerns have been raised about the interleukin (IL)-6 blocker tocilizumab and its potential negative impact on lipid profiles, although an increase in major adverse cardiac events (MACEs) was not demonstrated.24 Moreover, studies on the safety of Janus kinase (JAK) inhibitors (JAKi), such as the ORAL Surveillance study, suggest a higher risk of venous thromboembolic events (VTEs) and MACEs when using high doses of tofacitinib compared with TNFi.40 This risk seems notable in older individuals, smokers, and those with a history of coronary artery disease.40,52,53
Figure 1: Effect of disease modifying anti-rheumatic drugs on comorbidities in patients with chronic inflammatory rheumatic diseases
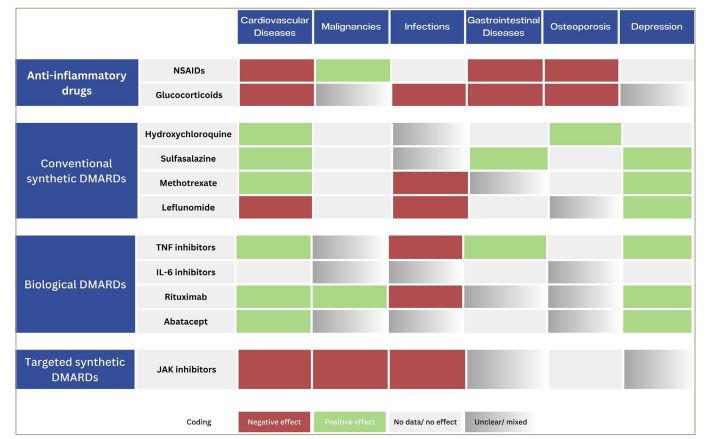
DMARDs = disease-modifying anti-rheumatic drugs; IL = interleukin; JAK = Janus kinase; NSAIDs = nonsteroidal anti-inflammatory drugs; TNF = tumor necrosis factor.
In return, some comorbidities may decrease the efficacy of some anti-rheumatic drugs. For instance, smoking may reduce the effectiveness of MTX, TNFi and abatacept, while it does not affect the response to rituximab and JAKi.54–56 As for obesity, it has been shown to reduce the efficacy of conventional synthetic DMARDs (cs-DMARDs), TNFi, and JAKi, while not affecting the outcome of rituximab therapy.54,56,57
Malignancies
The risk of developing a malignancy can vary depending on the CIRD, ranging from 1.5 times higher in patients with RA to 20 times higher in patients with primary Sjögren syndrome (pSS) compared with the general population.58 58,59 Haematological cancers, particularly lymphomas, are the most common malignancies across all patients with CIRDs.58–60
According to the National Cancer Institute, the most prevalent malignancies in the general population are breast, prostate, lung, and colon cancers.61 The cancer screening recommendations are reported in Table 1. Close monitoring for lymphoma is essential, especially in patients with Sjögren’s disease and with RA who have a markedly higher risk, with mucosa-associated lymphoid tissue (MALT) lymphoma and diffuse large B-cell lymphoma (DLBCL) being the most common types of lymphomas, respectively.58,59 It has been proposed that some features at Sjögren’s disease diagnosis can predict future lymphomagenesis, which may require a more intensive follow-up plan. These features include palpable purpura, salivary gland enlargement, low C4, leukopenia, cryoglobulinemia, monoclonal gammopathy, positive rheumatoid factor (RF), focus score and the total EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI).59
The incidence of lung cancer is increasing among individuals with RA, SLE, and SjS, partly attributed to smoking.60,62,63 In patients with RA, various factors could potentially contribute to the overall risk, encompassing attributes such as male gender, testing positive for RF or anti-citrullinated protein antibody, advanced age, smoking and interstitial lung disease (ILD).64,65 Potential for detection bias cannot be excluded in the CIRD population who undergoes comprehensive assessments. While targeted low-dose CT screening has been proposed, the currently available evidence does not substantiate extending this approach to encompass all patients with CIRD.65 As a preventive strategy, in conjunction with endeavors to promote smoking cessation, a recommendation is put forth for individuals aged 55–74 years with an elevated risk profile to undergo annual CT scans over 3 consecutive years.60,65 Tumour markers were deemed ineffective for lung malignancy screening; however, a positive correlation has been established between CA15-3 expression and an increased risk of developing ILD.66
Conversely, DMARDs like MTX, leflunomide, TNFi, tocilizumab, and rituximab contribute to 6–72% of drug-induced ILD, representing a minority of ILD cases.67 Interestingly, a study by Khan et al. suggested prior treatments for autoimmune disorders, like DMARDs and TNFi agents, might positively influence the patient’s response to anticancer therapies compared with individuals who haven’t received such previous treatments.68 Studies revealed no significant variance in lung cancer survival rates between individuals with CIRD and the overall population.68,69
Gynaecological malignancy screening in patients with CIRDs follows a similar approach to the general population, including biennial mammograms in women aged 50–74 years and an annual Pap smear.70,71 However, there is a need for heightened vigilance in individuals exposed to immunosuppressive drugs due to their increased risk for cervical premalignant lesions.71 For women up to 26 years old, herpes papillomavirus (HPV) vaccination is recommended and can be considered for young women with stable/inactive SLE and antiphospholipid syndrome (APS).60,70 However, caution should be exercised in those with a high-risk antiphospholipid profile.71
Screening for other malignancies should be guided by clinical suspicion and patient age, with 2–5 years of tight surveillance consisting of repeated tests if there are clinical suspicions.72 Positron emission tomography/computed tomography (PET/CT) may be considered in cases where unspecific systemic signs suggest the presence of neoplasms.72 Research conducted on serum tumour markers has failed to demonstrate their effectiveness in cancer screening.72
Earlier studies suggested that TNFi might be associated with an increased cancer risk, although more recent data from registries indicate the opposite.38,39,52,73 Also, data from the ORAL surveillance study found that the non-inferiority criterion of tofacitinib versus TNFi was not met regarding malignancies (Figure 1).40 The risk was identified only in patients above 65 years of age who were smokers. This has prompted the recent international recommendations for managing patients with RA and SpA advising assessing individual risk factors before prescribing JAKi.40
Infectious comorbidities and vaccination
Infectious diseases are a significant cause of morbidity and mortality in patients with CIRDs.37 The most prevalent infections among patients with CIRD are influenza, pneumocystis pneumonia (PCP), herpes zoster infections, and HPV.74,75 Most of these infections can be prevented through vaccination. Therefore, both pediatric and adult patients with CIRDs need to assess their vaccination status yearly and should receive routine vaccinations as per the National Immunization Program guidelines and EULAR recommendations.41,76
Screening guidelines for the general population prioritise the identification of sexually transmitted infections (STIs) and opportunistic infections, which is no different from the screening approach for individuals with CIRDs.77 Screening recommendations for higher-risk individuals include hepatitis B testing with hepatitis B surface antigen (HbsAg) tests, hepatitis C screening using anti-hepatitis C virus antibody tests for asymptomatic individuals aged 18–79 (confirmatory polymerase chain reaction testing if required), and non-treponemal and treponemal tests for syphilis screening with intervals determined by risk, while HIV testing is advised for individuals aged 15–65 with various risk factors using immunoassays and additional tests as necessary.33,34,78,79 Screening for latent tuberculosis (TB) infection is recommended for high-risk adults using Interferon-gamma release assay (IGRA) or tuberculin skin test (TST), with frequency based on risk level.42
In the CIRD population, several screening recommendations should be followed before initiating specific medications. Screening recommendations for latent TB, hepatitis B and C, HIV, and varicella-zoster virus before starting anti-rheumatic drugs are reported in Table 1.41
Prophylaxis against infections is achieved via vaccination. For the general population, vaccination calendars can be found on the CDC website according to age group.35 As for the CIRD population, non-live vaccines can be administered to both pediatric and adult patients with CIRD who are on GCs or DMARD therapy.36,37 Live-attenuated vaccines should be avoided in immunosuppressed patients, except for specific conditions like the measles, mumps and rubella (MMR) booster and varicella vaccination in pediatric patients.36 Pediatric patients with CIRD on MTX can receive MMR booster vaccinations, and varicella vaccination can be considered if they are varicella vaccination/infection-naïve and are on MTX or GCs, TNFi, anti-IL1, or anti-IL6 therapy.36 Yellow fever vaccination should be avoided in all immunosuppressed patients, regardless of age.36,37 Non-live seasonal influenza vaccination should be strongly considered for both pediatric and adult patients with CIRD treated with GCs or DMARDs.36,37 Pneumococcal vaccination with PCV10 or PCV13 is recommended for all non-vaccinated pediatric and adult patients with CIRD.75,76,80 Hepatitis A and B vaccinations should be given to at-risk patients with CIRD.37 HPV vaccination should be strongly considered in non-vaccinated pediatric patients with juvenile SLE and in other pediatric and adult patients with CIRD as per general population recommendations.37,76
The rheumatology team should assess the vaccination status and provide an individualised vaccination program to both pediatric and adult patients with CIRD.37 Vaccinations are considered safe, effective, and cost-effective in preventing certain infections in pediatric and adult patients with CIRD.76 However, vaccine efficacy may be reduced in some subgroups of patients with CIRD due to their immunosuppressed state. Therefore, vaccinations should preferably be administered during quiescent disease in both pediatric and adult patients with CIRD, if possible, 2–4 weeks before starting immunosuppression (especially B-cell depleting therapies).36,37 However, necessary treatments should never be postponed for vaccination.36
Interestingly, safety profiles of SARS-CoV-2 vaccines in patients with immune-mediated rheumatic diseases (I-RMD) were found to be reassuring and comparable to patients without I-RMD.81 Most patients tolerated the vaccines well, with only rare reports of I-RMD flare and infrequent reports of serious adverse events.81 These findings should provide reassurance, instilling confidence in the safety of SARS-CoV-2 vaccines for patients with I-RMD.81 Therefore, patients with CIRDs are strongly advised to receive any of the approved vaccines in their country.82
Additionally, it seems that patients with CIRDs do not face a higher risk of contracting SARS-CoV-2 than individuals without CIRDs, nor do they have a worse prognosis if they contract the virus.82 Nonetheless, there are concerns that individuals on certain immunosuppressive or immunomodulatory drugs may not mount an adequate protective response to COVID-19 vaccination.82 While data are not currently available to reliably identify who would benefit from a third primary dose of a SARS-CoV-2 vaccine, taking a precautionary position, some authorities recommend third primary doses in selected groups, and EULAR supports this approach.82 Additionally, concerns exist about the gradual decrease in protection vaccines provide against severe COVID-19 over time. Since insufficient time has passed to determine the expected levels of protection 4–6 months after the primary course, some authorities recommend booster doses, and EULAR supports this approach.82
As for the management of CIRD treatments during a COVID-19 infection, it is the role of rheumatologists to determine whether to maintain or discontinue immunomodulatory or immunosuppressive therapies and for those who have been vaccinated, treatment should continue unchanged. In contrast, those not vaccinated should consider the potential increased risk of severe COVID-19 when deciding on treatment.82 In patients with CIRDs who are not using immunomodulatory or immunosuppressive treatment, it is suggested that SARS-CoV-2 vaccination should precede the start of such therapy.82 For patients using rituximab or other B-cell-depleting therapies, scheduling the SARS-CoV-2 vaccination in a way that optimizes vaccine immunogenicity is recommended.82
Regarding the effect of CIRD treatments on susceptibility to infections, rituximab significantly hampers the generation of antibodies in response to vaccines, although it has minimal impact on T-cell responses.83 Similarly, medications like MTX and abatacept diminish the immune response to various vaccines and should be withheld before vaccine administration.83 TNF and JAK inhibitors generally reduce the antibodies produced after vaccination, but most patients, particularly those taking TNFi, still manage to achieve protective antibody levels.83 Conversely, therapies targeting cytokines such as IL-6, IL-12/23, and IL-17 do not appear to significantly influence the effectiveness of vaccines.83
Gastrointestinal diseases
The presence of GI complications in individuals with CIRDs is variable across different rheumatic diseases. For instance, clinically evident inflammatory bowel disease (IBD) in individuals with SpA is estimated to be around 7%.84,85 Coeliac disease (CD) affects approximately 2.9% of the overall CIRD population, particularly prevalent in patients with pSS and diffuse systemic sclerosis (SSc).86 Regarding GI motility disorders, achalasia (AC) and intestinal motility disorders (IEM) are the most frequently observed in patients with CIRDs.87
The screening process for GI comorbidities is similar in the general population and individuals with CIRDs, relying on symptom-based evaluation.7,86,88 However, certain CIRDs require a more thorough screening due to their heightened risk of specific GI issues.
In particular, an exhaustive screening for IBD is paramount in patients with SpA. This is due to the significant impact on treatment outcomes, where prompt diagnosis enhances the effectiveness of TNFi treatment and reduces the risk of disability.84 Techniques like digital chromoendoscopy and magnification colonoscopy are utilised to facilitate effective IBD screening, alongside a range of laboratory tests to assess markers like C-reactive protein, sedimentation rate, transferrin, ferritin, and vitamin B12 levels.85,88 Employing digital chromoendoscopy or magnification endoscopy aids in identifying and monitoring early lesions.89 IBD screening involves specific criteria, encompassing both major symptoms such as rectal bleeding, diarrhoea exceeding 4 weeks, and perianal disease, as well as minor indicators like prolonged abdominal pain, iron deficiency anaemia, and extra-intestinal manifestations such as aphthous stomatitis, fever, unexplained weight loss, family history of IBD, and vitamin B12 deficiency.88
A study conducted by Andréasson et al. investigated faecal calprotectin (FC) levels, commonly used in primary healthcare, to determine if patients should be referred for endoscopy in individuals with Sjögren’s syndrome.90 They found that an FC level exceeding 150 μg/g could indicate underlying GI conditions such as malignancy or IBD. This discovery suggests that FC could serve as a non-invasive biomarker for detecting GI inflammation, offering an alternative to relying solely on endoscopy for screening GI comorbidities in patients with CIRD. It is worth noting that elevated FC levels have also been observed in SSc and axSpA. However, using FC to screen for GI inflammation in patients with SpA seems to be associated with poor diagnostic properties (sensitivity 64%, specificity 73%), and FC levels are significantly affected by previous NSAID therapy.91,92
Furthermore, the screening process for CD entails evaluating IgA transglutaminase (TG) levels and conducting anti-endomysium testing for those with positive or borderline IgA TG results.86 Confirmation of CD is achieved through a duodenal biopsy.86 Notably, the early detection of CD is particularly vital in patients with pSS and diffuse SSc.86
Regarding GI motility disorders, particularly in patients with SSc, RA and SLE, oesophageal manometry is recommended to assess oesophagal function and pressure patterns.87
Gastric ulcers represent another GI comorbidity primarily linked to colonisation by Helicobacter pylori (H. pylori).93 A study by Lin et al. highlights that treating H. pylori in patients with peptic ulcer disease might elevate the chances of developing autoimmune disorders and IBD compared with untreated cases.93 Conversely, specific medications like GCs and NSAIDs exacerbate gastric harm, while proton pump inhibitors (PPIs) and COX-2-selective NSAIDs offer protection.94 Therefore, it is recommended to closely monitor patients receiving both GCs and NSAIDs, while also considering the use of PPIs and COX-2-selective NSAIDs.94
Osteoporosis
The prevalence of osteoporosis among patients with CIRD exhibits variability, yet it consistently remains elevated compared to the general population.27,28 The occurrence of osteoporosis in patients with SLE ranges from 1.4% to 68%, while instances of SSc are associated with a 23.6% prevalence of osteoporosis.27 Osteoporosis is often under-screened in high-risk populations like patients with RA and SpA due to the focus on treating the active disease and other comorbidities.28 Factors contributing to bone fragility in these diseases and requiring management include inflammation, sedentary lifestyle, menopause, corticosteroid use and intestinal inflammation.28,30
According to the US Preventive Services Task Force, screening recommendations for osteoporosis in the general population target all women aged 65 and above and postmenopausal women under 65 who are at higher risk.31 The most commonly used diagnostic test is central dual-energy X-ray absorptiometry (DXA) of the hip and lumbar spine.31
However, DXA provides quantitative assessments without considering qualitative aspects.28 CT scans may help, as they provide both morphological and density evaluation.28 Fauny et al. found that CT scans were as reliable as spine DXA for identifying patients at risk of vertebral fractures.28 The sensitivity of osteoporotic fracture risk assessment is enhanced when the Fracture Risk Assessment Tool (FRAX) and DXA scan are combined.32
In the CIRD population, the National Osteoporosis Foundation (NOF) recommends that patients with CIRD or adults taking GCs (daily dose ≥5 mg prednisone or equivalent for ≥3 months) should be screened for osteoporosis by central DXA regardless of their age. Also, using the lowest possible dose of GCs for the shortest period is recommended.30 Prophylactic vitamin D and calcium supplements are also recommended to enhance bone mass density (BMD) in GCs-induced osteoporosis.95,96 Considering the strong association between severe vitamin D deficiency and musculoskeletal disorders, it is advised to prescribe a daily dose of 1000 IU of vitamin D for individuals at a higher risk of deficiency.96 This supplementation regimen has been deemed safe and can be complemented with a loading dose or calcifediol treatment in specific patient groups to attain therapeutic levels of 25-hydroxyvitamin D.96
Supplementation alone falls short, necessitating comprehensive osteoporosis treatment: bisphosphonates (BPs) serve as the initial therapy choice, yet prolonged usage increases bone fragility and fractures.97 Hormone replacement therapies effectively reduce bone loss, but continuous use comes with substantial risks, such as cancer and thrombosis.97 Additional treatments like calcitonin relieve osteoporosis-induced bone pain, while RANKL (receptor activator of nuclear factor kappa-b ligand) inhibitors improve bone density and decrease fracture risk.97 Parathormone analogues rapidly increase bone density, necessitating co-administration with BPs, which have a slower onset. Hence. BPs are employed for maintenance, and the application of the anti-Sclerotin Antibody is restricted to specific high-risk patients.97 Recent findings indicate that concurrent use of bDMARDs and csDMARDs over a year minimizes BMD decline in the spine and hips.98 This integrated strategy not only improves joint scores and eases extra-articular symptoms, but also curtails widespread bone loss by optimizing disease activity reduction.98 Despite yielding moderate enhancements in BMD, biologic anti-rheumatic treatments have limited impact on fracture risk, underscoring their inability to replace osteoporosis-specific interventions.98
Under study are some emerging treatments encompassing stem cell therapy for the regeneration of osteoporotic bones, microRNA-based therapy for targeted interventions, and bone-specific targeting technology aiming to enhance treatment precision.97
Depression
Recent advancements in immunopsychiatry have provided a better understanding of the relationship between depression and inflammation, with elevated levels of specific inflammatory markers found in patients with depression or anxiety.99 Depression is twice as common in patients with RA compared with the general population, with approximately 17% of patients with RA experiencing major depressive disorder.99
In general, screening for depression is advised for various groups, including women during and after pregnancy, young and middle-aged adults, people of colour, those with low education levels, divorcees, unemployed individuals, those with chronic illnesses (including CIRDs), people with other mental health disorders, and those with a family history of psychiatric disorders. Several widely used depression screening tools include the Patient Health Questionnaire (PHQ) in its various forms (PHQ-2;4;8;9;15), the Hospital Anxiety and Depression Scales (for adults), the Geriatric Depression Scale (for older individuals), and the Edinburgh Postnatal Depression Scale (for pregnant and postpartum women).15,100,101
It is of the essence to diagnose depression early in patients with CIRDs to manage or refer such patients to psychiatrists. For example, the UK National Institute for Health and Care Excellence (NICE) guidelines for RA management includes psychological interventions to address fatigue, low mood, and social well-being.99 It has been proven that managing mental health and depression in chronic medical conditions improves treatment outcomes.99,102 Various tools, such as Beck Depression Inventory (BDI), Hospital Anxiety and Depression Scale (HADs), and Patient Global Assessment (PGA), are commonly used in rheumatology studies to measure mental health status and patient-reported outcomes.103–105 Additionally, non-pharmacological interventions are recommended to improve adherence, functional disability, pain, fatigue, goal setting and self-efficacy.102
Despite employing a treat-to-target strategy, many patients with CIRDs continue to face significant symptoms, particularly pain, and in cases of treatment resistance, depression can play a role.99 A study by Nagy et al. found that csDMARDs and bDMARDs were equally effective in enhancing patients’ quality of life.102 However, no significant differences were observed in their impact on anxiety and depression among patients with RA. It is important to note that failure to achieve complete disease control can result in physical limitations that exacerbate psychological and social issues.103 Therefore, the primary treatment objectives should focus on improving quality of life and reducing disability to avoid or limit depression.103
Consequently, optimizing treatment adherence is crucial and should be discussed through shared decision-making between healthcare providers and patients.102 Furthermore, it is essential to address non-inflammatory pain resulting from factors such as anxiety, depression, sleep disruptions, and psychosocial circumstances.106–108 This includes effectively managing additional sources of pain like fibromyalgia, mechanical pain, and neuropathic pain that coexist with the pain associated with CIRD.99,102
Other
Important concomitant pulmonary conditions associated with CIRDs are ILD and pulmonary hypertension (PH).109–111
ILD is the primary pulmonary concern in patients with RA, with approximately 60% of patients with RA exhibiting ILD on imaging.112,113 In contrast, the prevalence of ILD in patients with pSS varies widely, from 13% to 78%.114 Among patients with mixed connective tissue disease (MCTD), 50–80% have non-specific interstitial pneumonia (NSIP) on high-resolution computed tomography (HRCT).114 On the other hand, SLE has a lower incidence of ILD, affecting only 2–4% of patients with SLE compared with other autoimmune conditions.114 Various factors, including age, gender, disease duration, and antibodies to cyclic citrullinated peptides, contribute to the risk of developing ILD in patients with RA.112,113 Additionally, factors like smoking, unspecific interstitial pneumonia (UIP), emphysema and acute exacerbations are associated with an elevated mortality risk.112,113
PH can develop as a complication of CTDs like systemic SSc, MCTD, and SLE. Among these CTDs, SSc has the highest known prevalence of PH, affecting approximately 8–12% of patients with SSc.109
In clinical practice, the diagnosis of ILD primarily relies on HRCT findings due to practicality, given that diagnostic criteria encompass HRCT findings, lung biopsy, a combination of clinical presentation, and pulmonary function tests.110,113 To identify patients with RA who would benefit from HRCT screening, a study by Juge et al. proposed a risk score for subclinical RA-ILD incorporating four variables: sex, age at RA onset, RA disease activity assessed using DAS28-ESR, and the presence of the MUC5B rs35705950 genetic variant.115
For screening PH, a comprehensive approach is essential, involving physical examination, laboratory tests, pulmonary function tests, echocardiography and chest CT scans.109
There are conflicting findings regarding the impact of certain DMARDs like MTX, leflunomide, TNFi, rituximab, and tocilizumab on ILD progression in patients with RA.110,116 The overall evidence is inconclusive, but it suggests that some DMARDs, including MTX, leflunomide, TNFi, abatacept, and rituximab, may have potential benefits in preventing and treating patients with RA-ILD.110
The recommendations regarding the optimal screening method for each comorbidity or risk factor, the target population, the frequency of measurements and the management are summarized in Table 1. The impact of various DMARDs on the studied comorbidities is summarised in Figure 1.40,83,102,103,117–129
It is important to note that failure to achieve complete disease control can result in physical limitations, amplifying psychological distress and affecting the daily lives of patients.99,102,108 Nevertheless, this review provides a comprehensive summary of the most significant comorbidities and highlights some areas of unmet needs.
Conclusion
This narrative literature review summarizes the most recent recommendations spanning the past 6 years regarding the screening, prevention, and management of the six comorbidities documented in the core set data of the 2016 EULAR task force.7 The findings shed light on the uneven distribution of available information concerning managing comorbidities among different rheumatic diseases. Mainly, most publications seem to focus on RA and CVD, leaving a lack of clarity regarding managing other comorbidities in both RA and other CIRDs. As a result, there is an urgent need to consolidate and elucidate updated recommendations pertaining to the primary comorbidities observed in the most prevalent CIRDs. Additionally, the emergence of novel therapies introduces complexity, as each treatment uniquely influences the exacerbation or improvement of the mentioned comorbidities, prompting the application of personalized medicine.
Take-home messages
-
Comorbidities associated with CIRDs like CVD, malignancies, infections, GI diseases, osteoporosis and depression contribute significantly to the overall burden of the disease.1–3,5,7
-
Comorbidity screening in the general population follows established guidelines, but it is less standardized and requires more attention in the CIRD population.5,7
-
When selecting and managing DMARDs, consideration should be given to the impact on comorbidities.117–129
-
Individualized care and shared decision-making between healthcare providers and patients are vital for managing comorbidities in patients with CIRDs.7
-
Regular monitoring, appropriate screening and timely interventions can help reduce the burden of comorbidities and improve overall patient outcomes.7